- Comparative analysis of shear bond strength and quality of interface at novel bioactive material or Biodentine
Ivanka Dimitrova DMD, PhDa,* and Desislava Tsanova-Tosheva, DMDb
aAssociate Professor at Medical University – Sofia, Faculty of Dental Medicine, Department of Conservative Dentistry
bAssistant Professor at Medical University – Sofia, Faculty of Dental Medicine, Department of Conservative DentistryThis article is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pulp-capping materials, Composite material, Shear bond strength
Direct pulp capping (DPC) is a biological treatment method, indicated in reversible inflammatory diseases of the dental pulp (DP), in which a medication with appropriate physicochemical properties is applied at the site of communication with pulp and the goal is the initiation of reparative dentinogenesis and preservation of its vitality and functions [1]. Dental caries and its complications, complicated dental fractures, collisio pulpae might be the reason for direct pulp capping at timely and correct diagnosis of the reversible inflammatory pulp conditions.
The success of direct pulp capping depends on many factors: the type and stage of the inflammatory process; a correct diagnosis and a suitable treatment plan, age, localization of the ulcera, a microbial number after the caries removal, hemorrhagia control, the type of pulp capping agent, working in aseptic conditions, the experience of the clinician, etc. [2].
The utmost importance after direct pulp capping is the type of pulp capping agent used [3]. According to Bjørndal et al., the ideal pulp capping material should possess bioactive potential and induce the formation of a quality dentin bridge that hermetically seals the exposed site of the dental pulp and prevents bacterial penetration. For this purpose, calcium hydroxide has been considered as the “gold standard” in clinical dental practice for the of management DPC for many years [3]. However, many studies have reported that the dentine bridge after the use of calcium hydroxide (CH) contains tunnel defects [5-7].
The rapid development of materials science has led to the creation of a variety of calcium silicate cements (CSC) in the market. Calcium-silicate cements are bioactive materials with wide application in dental practice. They are applied for sealing of perforations, direct pulp capping, indirect pulp capping, apexification, apexogenesis, repair root- end filling, etc. [8]. The choice of a suitable calcium silicate cement depends on its mechanical properties, sustainability and type of clinical application.
Biodentine, (Septodont, Saint-Maur des Fosses, France) relatively new active biosilicate material, refers to the 3rd generation of calcium-silicate cements and is one of the main representatives of the bioceramics group [9, 10].
BioCalp Cap (Harvard, Germany) is a new, light curable resin modified bioactive material, that belongs to the 4th generation of biomaterial. It is a recently introduced material in dental practice. There is no information in the dental literature about its properties. More data is available for another representative of these generation- Theracal LC [11]. Two types of CSC of different chemical compositions were used in this study. Biodentine is synthesized from pure raw materials and is mixed with water liquid, chloride accelerator and a water- soluble polymer [12]. BioCalp Cap is made up of a Portland III type and HEMA monomer [13].
The other basic key factor for a good healing result after direct pulp capping is also the quality of the bond strength between the dentine and the capping material, as well as the bond strength between the capping material (PCM) and the composite resin material (CRM) that is used for the restoration [14]. Composite resin materials have been the most widely used for permanent type of restoration. According to Bawa et al. the success of DPC depends on the type of composite material chosen, its physicochemical properties and the quality of the adhesive bond with CSC [15]. The selected calcium silicate cement must be able to provide a quality adhesive bond with the restorative material as well. The qualitative bond strength with the restorative material provides a uniform redistribution of the masticatory stress on the border between them during the polymerization shrinkage of the composite and is a prerequisite for the durability of the restoration [16]. Current information in the literature regarding the most suitable time for the recovery with CRM over PCM is controversial [17].
There are no definite facts in the literature on the most appropriate time for final composite restoration on the pulp capping material and how this affects the interface between the two materials and the bond strength between them [17, 19, 20].
The purpose of this study is to compare and analyze the shear strengths of two pulp capping materials (conventional and hybrid) under the same conditions in terms of applying the same adhesive system and restorative material placed at different times: immediately after the setting of the pulp capping agent and postponed after 2 weeks. The first null-hypothesis was that the new hybrid CSC would provide a better quality adhesive bond compared to conventional cement Biodentine at both time intervals. The second hypothesis was that the different recovery times had effect on the shear strength values of the two materials tested. The third hypothesis was that neither the two time intervals nor the different types of CSC affect the qualities of an adhesive bond.
Material and methods
In the present study, 60 metal molds with a diameter of 5 mm and a height 2 mm were used. All of the procedures described below are carried out by one dentist and the purpose is to standardize of the conditions. The study was carried out in four groups of 15 samples in each as follows:
I group - Biodentine (Septodont, Saint Maur de Fosses; France) - immediately after its setting, a composite material is placed.
II group - Biodentine (Septodont, Saint Maur de Fosses; France) postponed, and 2 weeks after setting a composite material is placed.
III group - BioCal-Cap (Harvard, Germany) A composite material is placed immediately after it has been set.
IV group - BioCal-Cap (Harvard, Germany) postponed, and 2 weeks after setting a composite material is placed.
Preparation of the specimens
Biodentine (Septodont, Saint Mur de Fosses) is prepared according to the manufacturer's instructions: five drops of liquid are inserted in each capsule and the preparation of the mixture lasts for 30 seconds at 4000 rpm using a mixer by Capsules GC Silvermix (Japan). The mixed material is placed in the metal molds and the surface is smoothed with a spatula.
For the specimens of the I group, 12 minutes are required for the setting of the Biodentine, in conditions of moisture. Then the application of the universal adhesive system (Scotchbond 3M Espe, St. Paul, MN, US) in a thin layer is done, slightly dried and polymerized with a BlueDent Smart photopolymer lamp (Bulgaria) for 20 seconds.
For the third and fourth groups, a total of 30 samples, Biocal-Cap hybrid cement were prepared and used. The material is set by light polymerization for 40 seconds. For the samples of the III group, a subsequent surface is treated by applying and spreading a universal adhesive system (Scotchbond 3M Espe, St. Paul, MN, US) in a thin layer, slightly dried it and polymerized it with a BlueDent Smart photopolymer lamp (BG Light Ltd., Bulgaria) for 20 seconds.
Restorative procedures
For the placement of the composite resin material on the pulp capping materials, additional metal cylindrical molds (3/2 mm) are made, which are fixed to the samples and filled with Filtek Ultimate (3M, USA).
In the samples of I and III groups the application of CRM is placed immediately after the setting of the pulp capping material and in the other samples the application of the restorative material is postponed for two weeks. The last two groups of samples are stored at 37°C in thermostat conditions and moisture.
The so prepared monoblocks have undergone shear strength tests. Testing is carried out on an electro- mechanical bench for physico-mechanical tests Multitest 2,5-i (Mecmesin, UK).
Method
Test conditions for shear bond strength:
The strength test is carried out on the LMT-100 stand (LAM Technologies Electronic Equipment, Italy) of a special device for the implementation of shear forces in the adhesive layer of the sample.
The stand”s and software”s designs, as well as the device”s, provide reproducible performance of the load conditions of the test specimens. The precision of the measured displacement of the movable part of the structure is 0.001 mm. The speed of movement (load) of the test body can be set to 0.001 mm/s. The registered power is 0.1 N.
Scanning Electron Microscopy Examination
The selected destroyed test samples are subjected to further examination by Scanning Electron Microscopy (SEM) (Lyra TESCAN®) at 20 kV. The images of the selected materials are reviewed at different magnifications.
The statistical analysis has been done by the Mann-Whitney test and the Wilcoxon Signed Ranks Test.
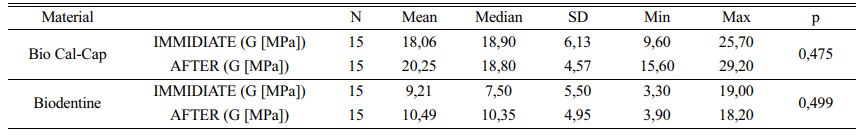
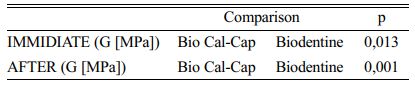
In both of the materials there is no statistically significant difference in results after immediate and postponed placement of the composite material. Nevertheless, in both of them there is a tendency for a slight increase in shear strength in samples with delayed application of the restorative material - Table 1.
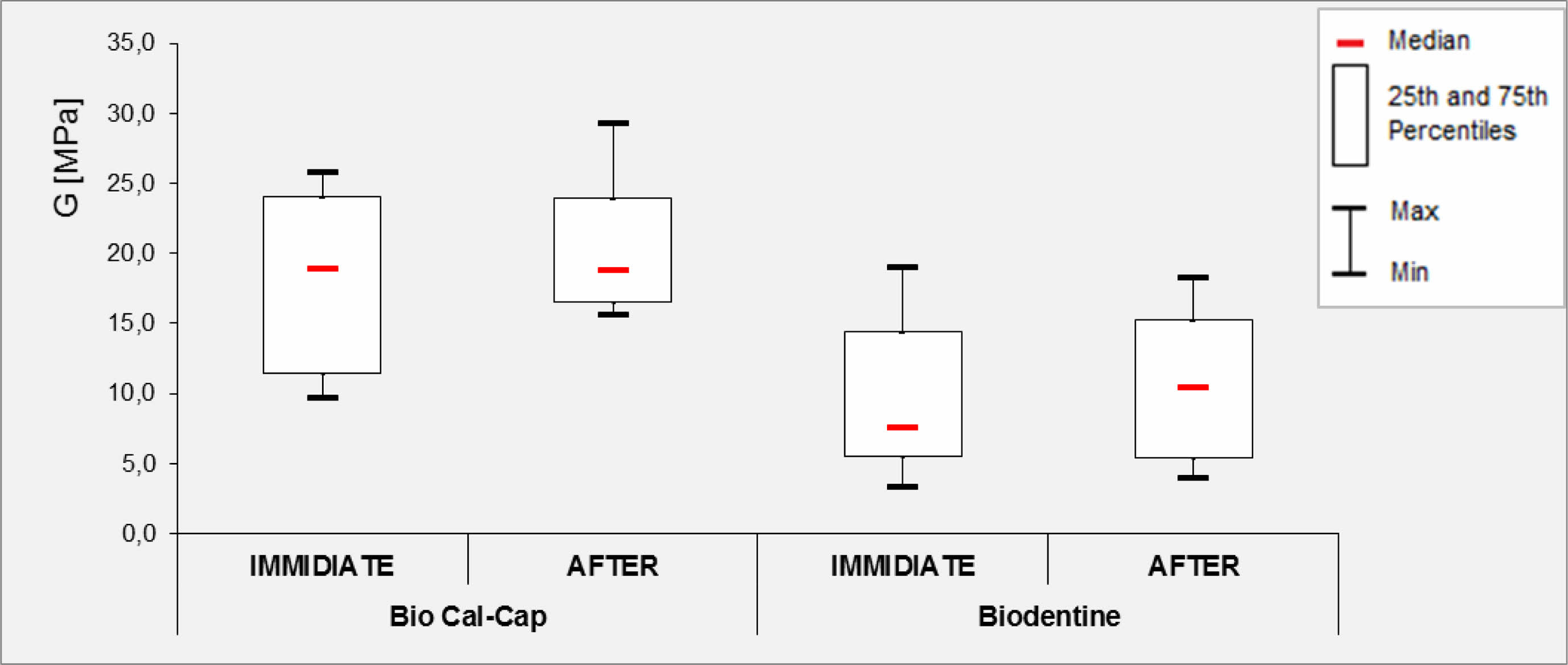
The diagram (Fig. 1) represents the distribution of the strength values for both materials. For the Biodentine, there is a tendency for displacement of the median value higher when postponed CRM placement is done, compared to the same in postponed placement. This shows that it is more appropriate for the composite material to be placed two weeks after the setting of the pulp capping agent. In the new material - BioCal-Cap there is the opposite tendency - the median value is shifted higher after immediate composite placement, which supports a one-step treatment approach.
In the comparison of the two materials there is a statistically significant difference in both the immediate placement of CRM and the postponed placement (p <0.05).
Analysis of the adhesive interface between the pulp-capping agent (PCA) and the composite resin material (CRM)
A good adhesive layer between composite resin and calcium-silicate cements is critical for a good healing result.
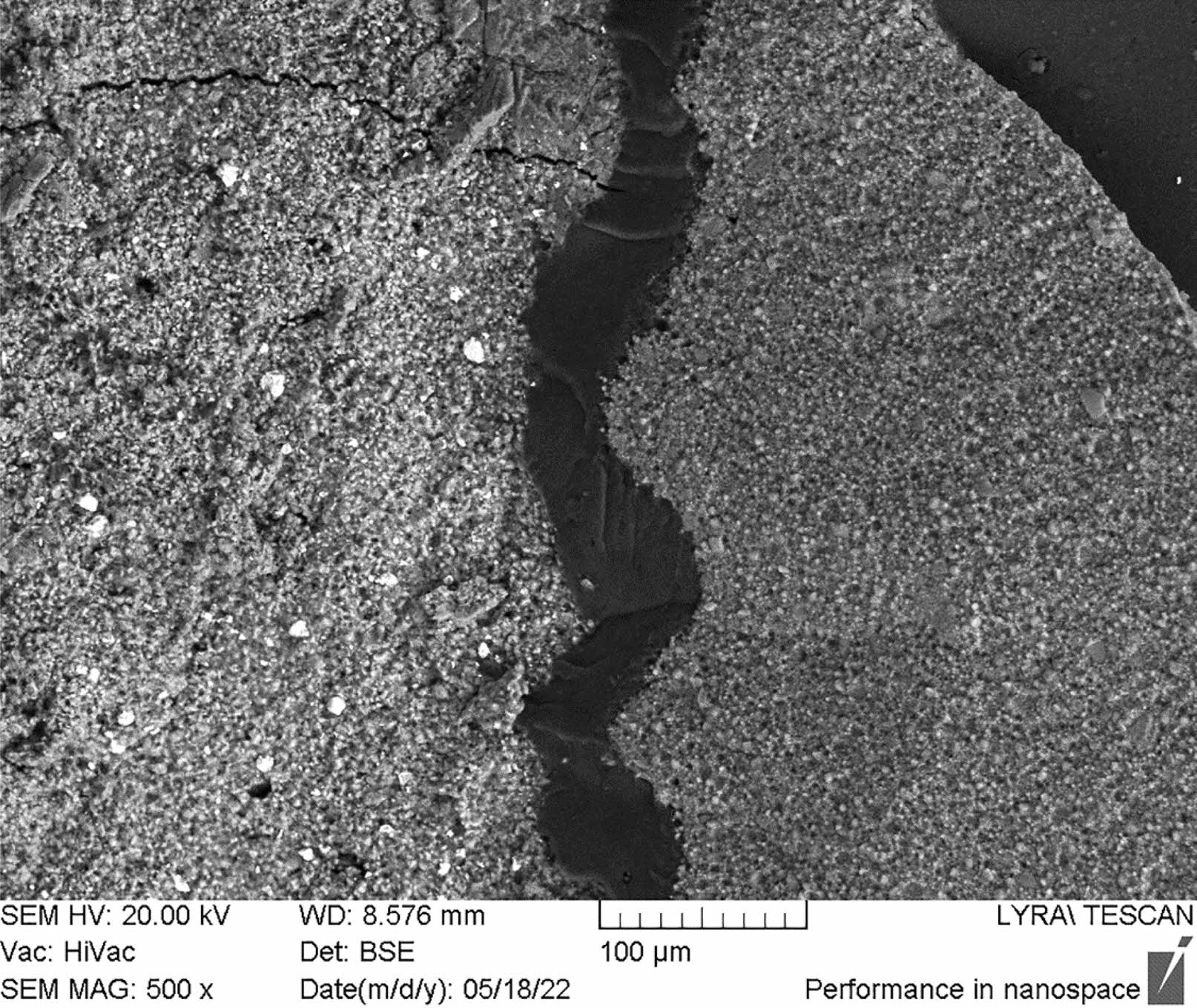
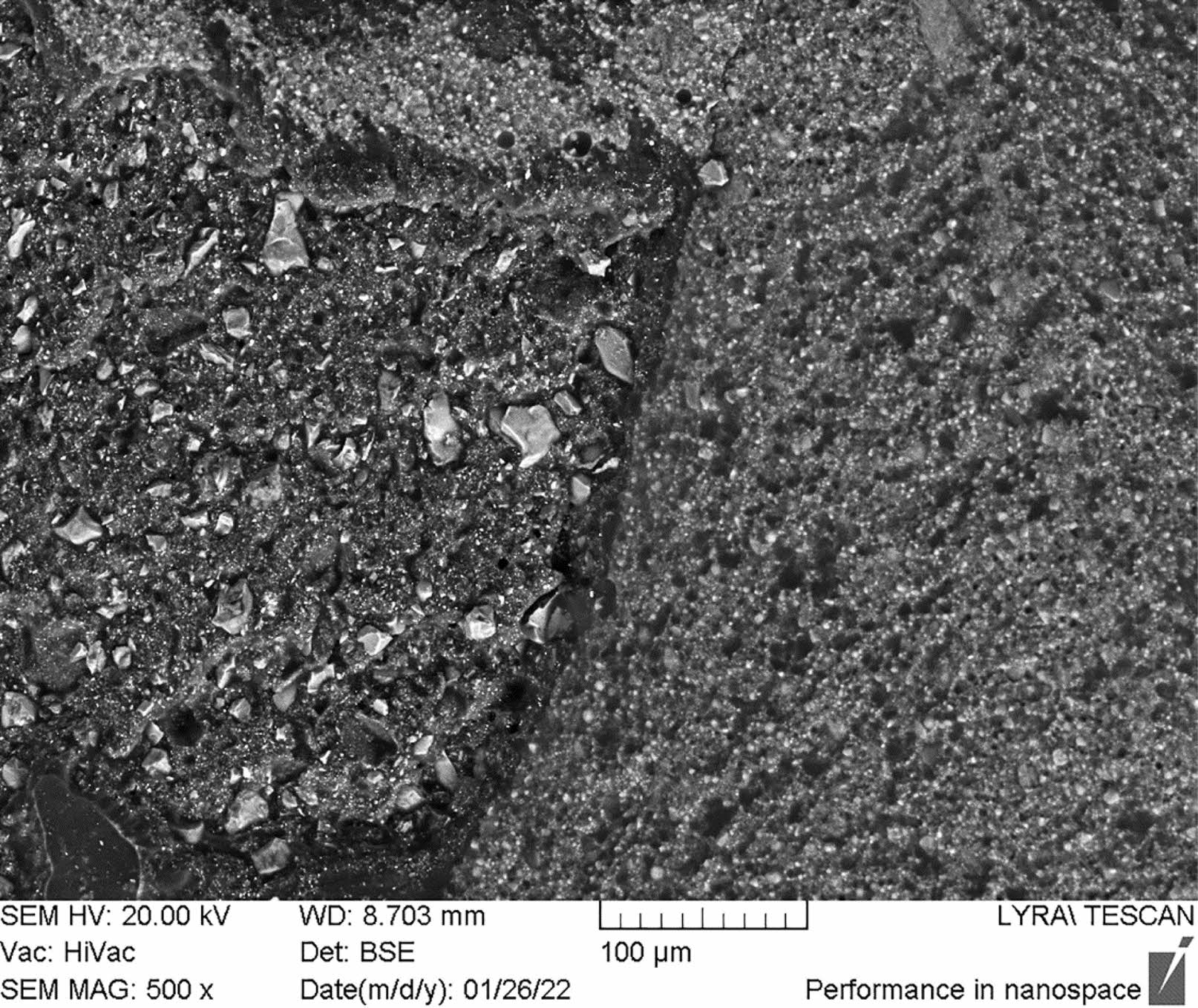
After debonding the selected samples from all groups were subjected to and evaluated using scanning electron microscopy. The aim was to assess the hybrid layer between the PCA and CRM. Its integrity is also a very important factor for the durability of the restoration.
In the dental literature is limited information on the interface between overlying composite resin restoration and calcium silicate cements. The integrity of the layer is important to the longevity of resin based restorations. It depends on the physicochemical properties of the used calcium silicate cements, composite resin and the type of adhesive system that forms the adhesive interface zone.
The investigated new hybrid cement preserved the integrity of this layer in all evaluated samples. As can be seen from the presented scanograms, this layer is homogeneous, properly structured, without the presence of microcracks and gaps, and has different thicknesses.
In all specimens with Biodentine, upon immediate restoration with composite material, cracks of different lengths and sizes were observed in the pulp capping material. Fewer cracks were recorded in the samples after delayed restoration with composite material. Biodentine has a high porosity which is causes by the spaces between the un-hydrated cement grains [21]. When a load is applied to porosity containing material the length of the crack increases in the direction of the pores according to Wang et al. [22].
The presence of a violation in the integrity of the pulp capping material also calls into question the good outcome of dentine wound treatment with Biodentine. This means that this material is not sufficiently resistant to load and changes in its integrity are registered. This conclusion is supported by the shear bond strength values found in this study for Biodentine. The bond analysis of Biodentine shows that even with delayed placement of restoration, the strength of Biodentine does not significantly increase. Fig. 2 Fig. 3 Table 2
|
Fig. 1 Distribution of strength values for Biodentine and BioCal-Cap. |
|
Fig. 2 Interface between Biodentine and composite resin material. Visible deep and long crack in Biodentine up to adhesive layer. |
|
Fig. 3 Interface between hybrid new cements and composite resin. Well presented and intact adhesive layer between new hybrid cement and composite resin material. |
Two different pulp capping materials are used in the present study: conventional (Biodentine) and hybrid (BioCal-Cap). Biodentine is calcium-silicate cement, that was introduced into the dental practice in 2011 as a bioactive material with a short setting time [24].
The other material used in the present study is the new BioCal-Cap (Harvard, Germany) hybrid cement introduced in 2019 and there is no information in the literature about its physico-chemical properties. The hybrid CSCs are modified with resin calcium-silicate cements, which are determined to materials have good biocompatibility and low solubility compared to the conventional ones [24]. The monomers added to their composition allow for their light polymerization, reduce the clinical time and allow the creation of a quality adhesion with the composite material [25].
Hybrid calcium-silicate cements and composite materials have similarities in their chemical composition. This allows them with bond chemically to each other.
The results reveal that in both of the materials, the adhesive bond strength after two-week placement of the CRM is stronger, although there are no statistically significant differences between immediate and delayed restorative material placement in both of the investigated materials. The new hybrid cement has 18,06 МРа strength after immediate placement which is lower than the value achieved after delayed placement of the composite-20.25 MPa.
Our findings show that the adhesive strength of Biodentine after immediate placement of CRM is 9.21 MPa and increases slightly to 10.49 MPa after postponed placement. These values are significantly lower than 17-20 MPa which are considered sufficient to resist the masticatory forces during function [26]. Similar data have been established by Salil et al. [27]. Other results on the adhesive strength (9.12 MPa) between Biodentine and CRM after immediate placement have also been reported by other authors [28]. But unlike us, they find a significant increase in the adhesive bond strength up to 19.55 MPa after a 24 hour postponed placement of the CRM, using a single step adhesive system. According to Kudva et al. the shear bond strength between Biodentine and Filtek™ Z350 XT was found to be 3.378-11,306 MPa at 12 min using three different types of universal adhesive systems by self-etch protocol [29]. The authors concluded that the effective bond strength values between Biodentine and universal adhesive systems are achieved by the self-etch procedure rather than acid etching
F. Hashem et al. [30] conclude that the placement of CRM should be postponed after 14 or more days after Biodentine placement, because there were significantly higher shear bond strength values in delayed probes than in those taken immediately. Unlike them we do not find a statistically significant increase with the adhesive bond strength in delayed placement of Biodentine. The authors mentioned above report a lack of significant differences in the quality of the adhesion between Biodentine and CRM when using a total etch and self etch adhesive protocol. Similar data on the impact of the adhesive protocol using a universal adhesive system on the adhesive strength has also been reported by others [31]. According to Cantekin K. [32] the type of the used composite material affects the adhesive strength between the pulp capping material Biodentine. They find that the bond between Biodentine and methacrylate composites is 17.7 MPa compared to 8.0 MPa for another composite - Silorane. In our study we used the methacrylate nanocomposite materials Filtek Ultimate and Biodentine but we did not find such high shear strength values for the conventional material in our research.
The quality of the adhesion between Biodentine and CRM is of great importance because this bioactive material is also used as a dentin substitute [33].
Unlike us, Carretero et al. find the bond strengths between Biodentine and CRM - Grandio after immediate and 24 hour postponed placement of the restorative material to be 13.65 and 19.16 MPa respectively. They use a single step adhesive protocol with a universal adhesive system Scotchbond Universal. Compared to them, we found significantly lower values when using the same adhesive system and protocol [34].
Hybrid calcium-silicate materials are relatively new materials and studies that apply to their adhesion to hard dental tissues and to restorative material are few.
The shear strength of the other hybrid cement studied by us was 18,06 МРа, when directly restored with methacrylate nanocomposite material Filtek Ultimate compare to 20,25 МРа, when delayed.
Similar data have been reported by Meenu et al. [35]. Their results relate to another hybrid cement - TheraCal LC. We will discuss and compare data with similar hybrid calcium-silicate cement on the market because we did not find any data on BioCal-Cap According to Deepa et al - the quality of the bond when Theracal LC is used with a universal adhesive system is 18.24 compared to 5.66 using Biodentine [36]. These data is similar to ours. We similar to S. Sismanoglu found higher adhesive bond values between the new hybrid PCM and CRM compared to the adhesive bond between Biodenine and CRM [37]. Higher values of the bond strength between TheraCal L and CRM have been found by others [38].
The good adhesion between pulp capping material and composite resin material is of great value for a reliable sealing of the dentine wound, preventing micropermeability, secondary microbial invasion and determining the good treatment outcome.
The analysis of the results clearly shows that the adhesive bond strength is dependent on the type of pulp capping agent. The appropriate selection of such material as well as the correct technique used the clinical protocol are important for achieving quality shear strength. This data clearly shows that there is no influence of the time factor of restorative material application for each of the studied calcium-silicate cements on the shear bond strength. The results confirm the first proposed hypotheses and reject the second and third one presented.
The analysis of the results clearly shows that the adhesive bond strength is dependent on the type of pulp capping agent. The adequate choice of such material and the accurately applied technique during the clinical protocol are important for achieving quality shear strength. In support of this, it is apparent that even two-week delay of composite placement over Biodentine, does not significantly alter the bond strength, under equal and standardized other conditions. In all specimens with Biodentine, upon immediate restoration with composite material, cracks of different lengths and sizes were observed in the pulp capping material. Fewer cracks were recorded in the samples after delayed restoration with composite material. The presence of a violation in the integrity of the pulp capping agent also calls into question the good outcome of treatment with Biodentine. Careful consideration should be given to the use of Biodentine as a pulp capping agent especially on teeth, the center of masticatory pressure.
This data clearly shows that there is no influence of the time factor of restorative material application for each of the studied calcium-silicate cements on the shear bond strength.
- 1. T. Dammaschke, J. Hist. Dent. 56[1] (2008) 9-23.
- 2. K. Cantekin and S. Avci, J. Appl. Oral. Sci. 22[4] (2014) 302-306.
-

- 3. L. Bjorndal, S. Simon, P.L. Tomson, and H.F. Duncan, Int. Endod. J. 52 (2019) 949-973.
-

- 4. A. Nowicka, G. Wilk, M. Lipski, J. Kołecki, and J. Buczkowska-Radlińska, Int. Endod. J. 41[8] (2015) 1234-1240.
-

- 5. M. Ulmansky, J. Sela, and M. Sela, J. Oral. Pathol. 1[5] (1972) 244-248.
-

- 6. J. Muruganandhan, G. Sujatha, S. Poorni, M.R. Srinivasan, N. Boreak, A. Al-Kahtani, M. Mashyakhy, H. Chohan, S. Bhandi, A.T. Raj, A. Zanza, L. Testarelli, and S. Patil. Appl. Sci. 11[7] (2021) 3045.
-

- 7. E. Nie, J. Yu, R. Jiang, X. Liu, X. Li, R. Islam, and M.K. Alam, Mater. 14[22] (2021) 6811.
-

- 8. M. Parirokh, M. Torabinejad, and P.M.H. Dummer, Int. Endod. J. 51 (2018) 177-205.
-

- 9. L. Jagadish and A. Krishna, IOSR J. Dent. Med. Sci. 18[12] (2019) 68-72.
-

- 10. N. Agrawal, V. Singh, A. Shrestha, M. Jaisani, I.K. Maharjan, and N. Jain, J. Nepal. Assoc. Pediatr. Dent. 3[1] (2022) 14-19.
-

- 11. L. Argueta-Figueroa, C.A. Jurado, R. Torres-Rosas, M.A. Bautista-Hernandez, A. Alhotan, and H. Nurrohman, Biomimetics 7[4] (2022) 211.
-

- 12. F. Shafiei, M. Doozandeh, F. Gharibpour, and A. Adl, Int. Endod. J. 52 (2019) 530-539.
-

- 13. Harvard, Germany
- 14. C. Rocha and G. Torres, In Modern Operative Dentistry. (Cham: Springer International Publishing; 2020)
- 15. P. Bawa, B. Bugade, A. Lavate, J. Jankar, A. Vernekar, and N. Hatte, World J. Pharm. Res. 9[13] (2020) 652-658.
- 16. N. Chaipattanawan, C. Manmontri, J.-C.F. Chiang, and P. Chompu-inwai, CM Dent J. 42[2] (2021) 44-58.
- 17. S.S. Oskoee, S. Kimyai, M. Bahari, Paria Motahari, M.J. Eghbal, and S. Asgary, J. Contemp. Dent. Pract. 12[6] (2011) 457-462.
- 18. Septodont, Saint-Maur des Fosses, France
- 19. D.F. Hashem, R. Foxton, A. Manoharan, T.F. Watson, and A. Banerjee, Dent. Mater. 30[3] (2014) 343-349.
-

- 20. P.J. Palma, J.A. Marques, M. Antunes, R.I. Falacho, D. Sequeira, L. Roseiro, J.M. Santos, and J.C. Ramos, Clin Oral Investig 25 (2021) 3131-3139.
-

- 21. J. Camilleri, L. Grech, K. Galea, D. Keir, M. Fenech, L. Formosa, D. Damidot, and B. Mallia, Clin Oral Invest. 18 (2014) 1437-1446.
-

- 22. J. Wang, L.J. Vandeperre, R.J. Stearn, and W.J. Clegg, J. Ceram. Process. Res. 2[1] (2001) 27-30.
- 23. A. Schmidt, E. Schafer, and T. Dammaschke, J. Adhes. Dent. 19[2] (2017) 129-135.
- 24. L. Pintado, E. Torre, M.D.S. Selayaran, R.V. de Carvalho, C.H. Zanchi, F.R.M. Leite, and A. Etges, J. Conserv. Dent. 21[1] (2018) 74-79.
-

- 25. C.S. Farah, V.G. Orton, and S.M. Collard, Aust. Dent. J. 43[2] (1998) 81-86.
-

- 26. M.A. Al-Sarheed, J. Contemp. Dent. Pract. 17[2] (2006) 9-16.
- 27. M. Salil, K.A. Gupta, B.P. Singh, M. Kaur, and A. Kumar, Dent. J. Adv. Stud. 8 (2020) 49-54.
- 28. M.E. Odabaş, M. Bani, and R.E. Tirali, Sci. World J. 62[6] (2013) 61-65.
- 29. A. Kudva, A. Raghunath, P.M.S. Nair, H.K. Shetty, V.F. D’Costa, and K. Jayaprakash, J. Conserv. Dent. 25[1] (2022) 54-57.
-

- 30. D.F. Hashem, R. Foxton, A. Manoharan, TF. Watson, and A. Banerjee, Dent. Mater. 30[3] (2014) 343-349.
-

- 31. J.H. Shin, J.H. Jang, S.H. Park, and E. Kim, Int. Endod. J. 40 (2014) 1210-1216.
-

- 32. K. Cantekin, J. Clin. Pediatr. Dent. 39 (2015) 143-148.
-

- 33. H. Zhou, Y. Shen, Z.-J. Wang, L. Li, Y.-F. Zheng, L. Hakkinen, and M. Haapasalo, Int. Endod. J. 39[4] (2013) 478-483.
-

- 34. V. Carretero, L. Giner-Tarrida, L. Penate, and M. Aregui, Coatings 9[12] (2019) 783.
-

- 35. G.S. Meenu and W. Palak, Endodontology 32[1] (2020) 14-19.
- 36. V.L. Deepa, B. Dhamaraju, I.P. Bollu, and T.S. Balaji, J. Conserv. Dent. 19[2] (2016) 166-170.
-

- 37. S. Sismanoglu, Z. Yildirim-Bilmez, A.T. Gurcan, and B. Gumustas, J. Adhesion Sci. Technol. 36 (2022) 1833-1846.
-

- 38. H. Jeong, N. Lee, and S. Lee, J. Korean Acad. Pediatr. Dent. 44 (2017) 200-209.
-

 This Article
This Article
-
2023; 24(2): 353-358
Published on Apr 30, 2023
- 10.36410/jcpr.2023.24.2.353
- Received on Dec 19, 2022
- Revised on Feb 13, 2023
- Accepted on Feb 23, 2023
 Services
Services
Shared
 Correspondence to
Correspondence to
- Ivanka Dimitrova DMD, PhD
-
Associate Professor at Medical University – Sofia, Faculty of Dental Medicine, Department of Conservative Dentistry
Tel : +359 887 838 973 - E-mail: vanja_ves@abv.bg



 Copyright 2019 International Orgranization for Ceramic Processing. All rights reserved.
Copyright 2019 International Orgranization for Ceramic Processing. All rights reserved.