- Study on the effect of gait cycle improvement with robot assisted rehabilitation
Sun Qianga,* and Miao Qib
aChuzhou Polytechnic, Chuzhou, 239000, China
bThe First People's Hospital of Chuzhou, Chuzhou, 239000, ChinaThis article is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
The classification based on flat training is proposed with training of exoskeleton lower limb rehabilitation robot and the flat walking training robot. The method from the system composition, training characteristics, indications, from the subacute phase and chronic phase of rehabilitation training, in the subacute stage, 60 cases were selected, including 33 patients with hemiplegia and 27 normal patients who underwent rehabilitation training, after 6 weeks of robot training for chronic hemiplegia, training outcome scores higher than 9 on the Berg balance Scale and shorter course of illness were highly correlated with improved walking ability
Keywords: Gait cycle, Berg balance Scale
At first, rehabilitation medicine only focused on reha- bilitation treatment methods and neglected rehabilitation training, and the research on rehabilitation evaluation was also insufficient and even evaluation methods were not standardized [1]. Generally, the evaluation param- eters and control parameter values under normal con- dition were not given in the various evaluation methods of limb motor function adopted, and physicians com- pletely relied on subjective judgment for limb dynamic evaluation. In most cases, the physicians make a com- prehensive evaluation of physiotherapy effect through visual observation, which is not accurate and normative. As a result, for the same case, due to subjective bias, different physicians would come up with different evaluation results and give different rehabilitation treat- ment plans. Therefore, standard physiotherapy techniques must be developed to carry out rehabilitation training [2]. The development of modern robotics provides a new method for rehabilitation training, and the robot used for rehabilitation training is the successful appli- cation of robotics in rehabilitation medicine [3]. The main function of rehabilitation training robot is to help patients complete various motor function recovery train- ing, such as neck motor training, spine motor training, arm motor training, walking training, etc. [4]. At present, the commonly used lower limb rehabilitation robots can be divided into two driving modes: leg driving and foot driving. The leg-driven robot is exoskeletal, the main feature of this robot is a bionic exoskeleton struc- ture similar to human legs, when in use, the exoskel- eton mechanical leg is worn on the lower limb of the human body, and the normal gait is simulated according to the motion trajectory of the lower limb joints in the gait cycle [5]. Lokomat gait rehabilitation training robot is a typical representative of exoskeleton robots and has been widely used in clinical practice [6]. In 1999, Lokomat successfully developed a set of robots that can assist patients with lower limb movement disorders to automatically perform weight reduction walking training on the medical running table, which is mainly composed of gait orthotics, weight support system and running table [7]. Chen et al. believed that sensors installed at the joint of the mechanical leg would feed back the angle and driving force of the joint to the computer control software to set the individual gait pattern and training scheme; Feedback can be provided to patients through virtual reality technology to improve the initiative of patients to participate in training [8].
Plantar driven gait rehabilitation training robots, such as HapticWalker, are used to train patients' feet by driving the movements of their ankle joints during simulated walking. They are usually combined with weight-loss walking training. Its main structure is a pair of movable pedals which can move according to a certain trajectory. During the training, the patient stands on the pedal and completes the walking action driven by it [9]. Yongfeng et al. proposed that this robot has a drive system composed of a motor, planetary gear, crank mechanism and pedals, it can produce a regular elliptical trajectory, which is used to simulate the ankle joint motion trajectory in walking. The system can provide a variety of training modes, such as active, passive and damping, according to the needs of patients, but it cannot simulate the plantar pressure and the motion trajectory of the hip and knee in the walking cycle [10, 11].
According to the characteristics of auxiliary walking training, the exoskeleton lower limb rehabilitation robot can be divided into two categories: Treadmill – based exoskeleton robot and over-ground walking exoskeleton Robot [12].
Treadmill – based exoskeleton robot:
System composition
Lokomat is the world's first weight-loss walking training robot that combines a treadmill with an exo- skeleton robotic leg. The training robot is mainly com- posed of a suspension weight reduction support system, lower extremity exoskeleton gait orthotics and running platform and its control system. The two mechanical legs of the gait corrector include a power drive device and a sensitive sensor. When using, the mechanical leg is bound to the lower limb of the human body, and the mechanical leg simulates the normal gait and drives the legs to swing in coordination to complete the walking training.
Training characteristics
Each exoskeleton mechanical leg is driven by two motors, which drive the screw nut to rotate and push the mechanical leg to swing to complete the motion of the hip joint and knee joint with 4 degrees of freedom. The hip and knee can be trained accurately according to the parameters set by the system software, and the active and passive training can also be conducted according to the patient's own level of motor function. The sensor installed on the leg can measure the driving torque, joint Angle and other information, and feed back to the control system in real time, so as to evaluate and guide the training status online, and set the personalized training program. Its virtual reality design can not only give visual stimulation, but also increase the interest and participation of training to achieve better results.
Indications
In recent years, tablet training-based rehabilitation robots, represented by Lokomat, have been widely used in clinical applications, their indications include patients with lower limb motor dysfunction such as stroke, spinal cord injury, cerebral palsy, multiple sclerosis and Parkinson's disease. In the process of use, the force of the mechanical leg will be detected in real time. When the robot is subjected to certain resistance, in order to protect the safety of patients, therefore, patients with high lower extremity muscle tension and poor cognitive function are likely to cause the mechanical arm to stop working during the training, which should be used with caution.
Over-ground walking exoskeleton Robot
System composition
Ekso (EksoBionics, USA) is a typical flat walking training robot/ over-ground walking exoskeleton Robot. The robot consists of an exoskeleton wearing device and a special walking stick. Hydraulic cylinders and batteries are integrated into the backpack to power the robot, and the special crutches not only have control buttons but also maintain the trainer's balance.
Training characteristics
The patient wears an exoskeleton, and a power device integrated into the backpack drives the lower limbs to move from sitting to standing, from standing to sitting and walking, while maintaining balance and controlling movement with walking-aids such as a cane. It allows patients to perform targeted functional impairment training, such as sitting to standing. These mobile devices can also assist patients with activities of daily living and improve their quality of life [13].
Indications
The flat level walking training robot/ over-ground walking exoskeleton robot was first used to assist patients with complete spinal cord injury to walk. Due to the authenticity and mobility of the training scene, it has also been used in the research and clinical practice of the rehabilitation of stroke patients in recent years. When this kind of robot conducts walking training, the patient needs to participate actively to make the leg enter the swinging phase; As there is no suspension weight loss device to assist, higher requirements are put forward for the user's trunk control ability and balance function, and patients with poor cognitive and balance coordination functions should be cautious [14].
Repeated training of a large number of normal movement patterns in the affected limb can expand the cortical areas that innervate the movement of the limb, enhance the efficiency of neurotransmission, and facilitate the establishment of normal movement procedures and improve neuroplasticity. Traditional rehabilitation, exer- cise and functional training programs are formulated according to patients' conditions through rehabilitation evaluation. In addition, targeted exercise training stimu- lates nerve endings and muscle activity to promote the recovery of the nervous system. This method relies on the physical strength of rehabilitation therapists, the training intensity is limited, and it is difficult to achieve a large number of repeated precision training. In order to solve these problems in the rehabilitation process, the exoskeleton lower limb rehabilitation robot was brought in to achieve high intensity, targeted, repeatable and task-oriented training, and reduce the heavy physical labor of therapists. Rehabilitation robot assisted therapy can not only free up the therapist's labor force, but also enable patients to achieve early walking training, pro- viding high intensity, repetitive precision movement control [16].
Patients with early hemiplegia have poor standing balance, lower limb strength and lack of walking ability. The lower limb rehabilitation robot can not only assist patients to stand as early as possible, but also provide repeated normal gait stimulation to help patients recover. A prospective randomized controlled trial demonstrated that the combination of robotic gait training with traditional gait training improved walking function in patients with early bedridden hemiplegia. Several studies have demonstrated that robots combined with traditional rehabilitation therapy can significantly improve the recovery of patients' walking ability. Robot-assisted walking training can also improve the patient's static and dynamic balance function. A randomized controlled study showed significant changes in patients' peak oxygen uptake after robot-assisted training, sug- gesting that walking training robots have the potential to improve patients' cardiopulmonary function [17].
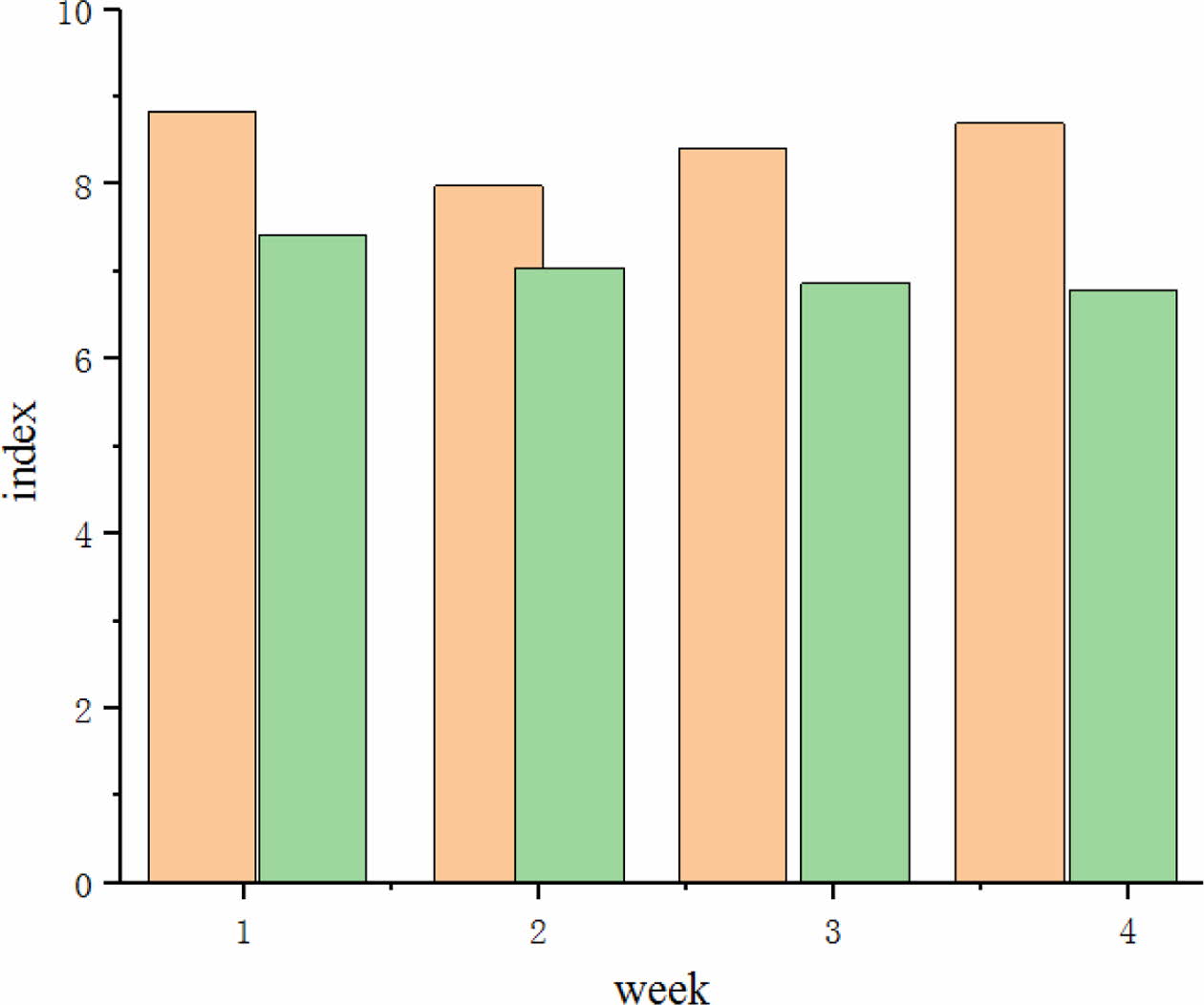
A 4-week robot walking training was conducted in 60 cases, including 33 patients with hemiplegia and 27 normal patients who passed rehabilitation training respectively, results as shown in Fig. 1, a Berg balance scale score higher than 9 and a shorter course of disease were highly associated with improved walking ability.
From the results of the study, after treatment 8 suba- cute hemiplegia patients trained with a robot showed improvement in the walking speed and functional walking ability of the patients. Two other studies also found that robot training had a positive effect on improving walking speed in subacute patients. One study compared robot-assisted walking training with traditional training, and after four weeks of training, there was no significant difference in walking speed and walking endurance between the two groups, but the functional walking ability of the experimental group was significantly improved. This is also reflected in the positive therapeutic effects of the two types of robots in patients with early hemiplegia [18]. After stroke patients enter the chronic phase, although the recovery of neurological function is slowed down, the patients' functional activity can still be improved after appropriate rehabilitation.
A case study of a patient with chronic hemiplegia who underwent six weeks of robot training showed significant improvements in walking endurance, speed, and walking ability. Surface electromyography (EMG) showed that the motor unit activity of the vastus medialis muscle was significantly increased. Other researchers have not only found that robot training improve the walking ability of patients with chronic hemiplegia, but also positively affect their balance function and even their confidence in balance. Active training with robot can also help patients with severe lower limb dysfunction to recover their walking ability. The high-speed robot training improved the patients' walking ability and balance function more than the traditional walking training. When functional electrical stimulation was combined with robot training, walking function and balance ability of patients tended to be improved compared with robot training alone, but there was no statistical significance. Adding functional electrical stimulation to robot training can improve patients' active participation without side effects.
|
Fig. 1 Berg balance Scale score. |
The rehabilitation training of exoskeleton lower limb rehabilitation robot and the flat walking training robot based on flat training are proposed. Training outcome scores higher than 9 on the Berg balance Scale and shorter course of illness were highly correlated with improved walking ability. These two types of exoskel- eton lower extremity rehabilitation machines have been applied in the rehabilitation of stroke patients in the subacute phase and chronic phase, and found to have certain clinical significance in the improvement of gait and balance function of stroke patients, as well as the recovery of lower extremity motor function.
- 1. Q.L. Li, Y. Song, and Z.G. Hou, Neural Process Lett. 41[3] (2015) 371-388.
-

- 2. I. Akgün, E.E. Avc, E. Timurta, I. Demirbüken, and M.G. Polat, Gait Posture 81[4] (2020) 8.
-

- 3. H.Y. Huang, I. Farkhatdinov, A. Arami, M. Bouri, and E. Burdet, IEEE T Bio-Med. En. 99 (2020) 1-1.
- 4. T. Kudo, CIRC J, 83[9] (2019) 1840-1841.
-

- 5. M. Hennes, K. Bollue, H. Arenbeck, and C. Disselhorst-Klug, Biomed. Tech. 60[3] (2015) 193-197.
-

- 6. J.Y. Kim, J.J Kim, K. Park, Int. J. Precis. Eng. Man. 20[10] (2020) 1767-1775.
-

- 7. J. Wang, X. Chen, J. Zhao, and W.W. Zhang, J. Vasc. Surg. 74[3] (2021) E58-E59.
-

- 8. Y.K. Chen, Sensor Lett. 15[1] (2017) 56-59.
-

- 9. Y. Lao, B. Jia, P. Yan, M. Pan, X, Hui, J. Li, W. Luo, X. Li, J. Han, P. Yan, and L. Yao, Medicine 98[50] (2019) e18324.
-

- 10. S. Gupta, P. Gupta, and A. Rajwanshi, Cytopathology 31[6] (2020) 616-618.
-

- 11. X. Zhao, W.H. Chen, B. Li, X. Wu, and J. Wang, Rev. Sci. Instrum. 90[12] (2019) 125112.
-

- 12. H.T. Lee, H.L. Roh, and Y.S. Kim, J. Phys. Ther. Sci. 28[2] (2016) 626-631.
-

- 13. M. Mundt, W. Thomsen, T. Witter, A. Koeppe, S. David, F. Bamer, W. Potthast, and B. Markert, Med. Biol, Eng. Comput. 58[1] (2020) 211-215.
-

- 14. B. Satheesh, Turcomat 12[5] (2021) 1551-1558.
-

- 15. P. Caruso, M. Ridolfi, G. Furlanis, M. Ajčević, M. Semenic, R. Moretti, M. Naccarato, and P. Manganotti, J. Neurol. Sci. 405 (2019) 116427.
-

- 16. A.Y. Omorou, H. Achit, M. Wieczorek, J. Pouchot, B. Fautrel, A. C. Rat, and F. Guillemin, Qual. Life Re. 28[5] (2019) 3047-3054.
-

- 17. J.V. White, M. Conte, A. Bradbury, P. Kolh, F. Dick, R. Fitridge, J. Mills, J.-B. Ricco, and K. Suresh, J. Vasc Surg. 69[6] (2019) 3S-125S.e40.
-

- 18. D. Selva, B. Nagaraj, D. Pelusi, R. Arunkumar, and A. Nair, Algorithms 14[8] (2021) 224.
-

- 19. Z.A. Abedali, A.C. Calaway, T. Large, M.O. Koch, J.E. Lingeman, and R.S. Boris, J. Endourol. 34[2] (2020) 163-168.
-

- 20. F. Schuur, M. Mehrizi, and E. Ranschaert, Eur. Raniol 3[8] (2021) 6021-6029.
-

- 21. A. Esquenazi and M. Talaty, Phys. Med. Reh. Clin. N 30[2] (2019) 385-397.
-

 This Article
This Article
-
2022; 23(2): 154-157
Published on Apr 30, 2022
- 10.36410/jcpr.2022.23.2.154
- Received on Aug 26, 2021
- Revised on Sep 25, 2021
- Accepted on Sep 27, 2021
 Services
Services
Shared
 Correspondence to
Correspondence to
- Sun Qiang
-
Chuzhou Polytechnic, Chuzhou, 239000, China
Tel : +0550-3854658 Fax: +0550-3854658 - E-mail: sunqiang228@126.com



 Copyright 2019 International Orgranization for Ceramic Processing. All rights reserved.
Copyright 2019 International Orgranization for Ceramic Processing. All rights reserved.